trending topics
market reports
-
MEDICAL JAPAN 2025 OSAKA Returns to Showcase Global Innovations
2025-02-17
-

Visit MEDICAL JAPAN 2023 TOKYO and take full advantage of the business opportunities!
2023-09-01
-

US to distribute 400 million free N95 masks at CVS, Walgreens in COVID fight
2022-01-21
-

Ethiopia receives additional 2.2 mln doses of Chinese-donated COVID-19 vaccines
2022-01-21
-
Hong Kong researchers say they develop novel material able to kill COVID-19 virus
2022-01-14
-

10 million more Chinese doses on way for Kenya
2022-01-14
-

Sino-African ties on track for a brighter future
2022-01-07
-

Efforts urged to boost COVID-19 vaccine production capacity in poor countries
2022-01-07
-

UAE approves Sinopharm's new protein-based COVID-19 vaccine
2022-01-07
-

UAE approves Sinopharm's new protein-based COVID-19 vaccine
2022-01-07
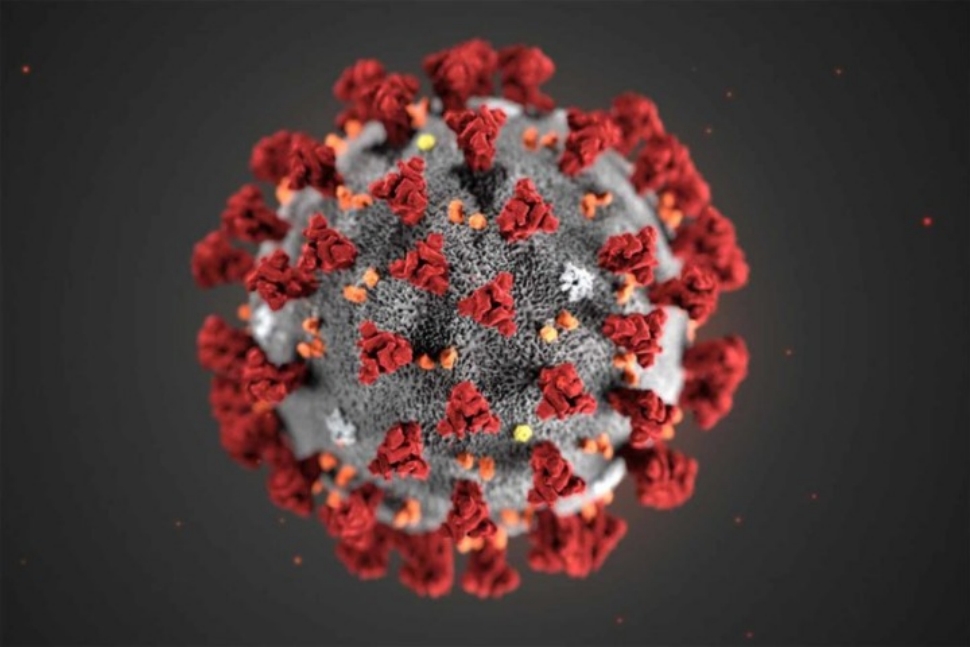
How Effective Will COVID-19 Vaccines Be?
2020-12-15

This article is part of Harvard Medical School’s continuing coverage of medicine, biomedical research, medical education and policy related to the SARS-CoV-2 pandemic and the disease COVID-19.
The success of a COVID-19 vaccine will depend on its efficacy and will also hinge on how fast and widely it can be delivered, the severity of the pandemic and the public’s willingness to be immunized, according to a study by Harvard Medical School researchers based at Massachusetts General Hospital.
The study, published in Health Affairs, finds that far more investment is needed to ensure that approved COVID-19 vaccines can be produced and distributed efficiently and that more must be done to promote the public’s trust in immunization and its willingness to continue practices that slow the spread of SARS-CoV-2. Rochelle Walensky, an HMS professor of medicine and chief of the Division of Infectious Diseases at Mass General, is senior author on the study.
Billions of dollars have been spent on developing COVID-19 vaccines, and preliminary evidence suggests that several candidates appear to be extraordinarily effective.
“But there are lots of ways to think about the effectiveness of a vaccine,” said Walensky.
She teamed with A. David Paltiel, professor of public health at the Yale School of Public Health, and several other colleagues to create a mathematical model that assessed how factors beyond efficacy might influence how well a COVID-19 vaccine will thwart the disease. Those factors included:
- How fast and broadly can the vaccine be produced and administered. Some candidate vaccines pose logistical challenges, such as needing to be stored in ultra-cold freezers or requiring two doses, spaced weeks apart.
- The portion of the population is willing to be vaccinated. National surveys suggest that as few as 50 percent of Americans say they will receive a COVID-19 vaccine.
- The severity of the pandemic when a vaccine is rolled out. The proportion of infections a vaccine is able to avert is directly related to the public’s willingness to engage in mitigation behaviors, such as wearing masks and social distancing.
The mathematical model they employed considered how these factors would influence the impact of vaccines of varying levels of efficacy.
“We found that infrastructure will contribute at least as much to the success of the vaccination program as will the vaccine itself,” said Paltiel. “The population benefits of vaccination will decline rapidly in the face of manufacturing or deployment delays, significant vaccine hesitancy or greater epidemic severity,” he added.
To help ensure a vaccination program’s success, Walensky said that a significantly greater investment in infrastructure to deliver COVID-19 vaccines is needed.
Moreover, powerful public messages and on-the-ground implementation strategies at the local level are also necessary to help overcome skepticism about vaccines, especially in underserved populations.
The Health Affairs study showed that even a highly effective vaccine will struggle to control COVID-19 if infection rates continue to rise.
“If I have a cup of water, I can put out a stove fire. But I can’t put out a forest fire, even if that water is 100 percent potent,” said Walensky, emphasizing the public’s role in keeping the infection rate low by wearing masks and practicing social distancing.
“We’ll get out of this faster if you give the vaccine less work to do,” she said.
(Havard Medical School)



 My Member
My Member Message Center
Message Center